There are several causes of yellow nails, some cosmetic in etiology and others indicative of an underlying medical issue and so it is important to understand when to see a physician.
One of the most common causes of yellow nails is from secondary staining from nail lacquer. Because the porosity of the nail is variable, certain individuals who inherently have more porous nails are more prone to pigment migration and thus secondary yellowing. Another common cause of polish induced nail yellowing is from the polish remover. Polish remover dissolves polish resulting in the migration of pigments that then can leach into the nail plate causing yellow discoloration. Theoretically the longer the soak, the more leaching that will potentially occur. The last factor related to polish has to do with the dye content of the polish. Not all polish dyes are alike. Generally, the darker the color, the more the pigment has an opportunity to migrate and leach into the nail plate to cause yellowing. While darker colors tend to be the culprit more often, this phenomenon can also occur with lighter colors as well. Yellowing from polish is not a brand related phenomenon. Yellowing is an issue that can occur with all nail polish brands.
How do we distinguish polish induced yellowing from other causes of nail yellowing?
When the cause is purely from polish, the nail will be healthy looking and intact but have a yellow hue throughout. The surface will be smooth and a normal thickness as opposed to fungal nails where there is thickening or subungual (under the nail) crumbling. And importantly, there will be a history of prior polish application.
How to treat?
Polish induced nail yellowing is a cosmetic issue. There are two options as far as treatment. The first is to take a nail polish holiday and to try to lighten the nail. Alternatively, the nail can be camouflaged with additional polish. For those who want to treat, severe stains can be lightened by using a dilution of Hydrogen Peroxide. This at home remedy can be made by combining three to four tablespoons of Hydrogen Peroxide and 1/2 cup of water and mix well, then soak nails for 2 minutes. Using a soft toothbrush, gently scrub the surface of the nails. Rinse with water. Repeat 2-3 times per week as needed. Alternatively, you can use a whitening toothpaste as these are formulated with Hydrogen Peroxide. The Dr. DANA Nail Renewal System is great for lightening discolored nails. Step 01 contains Glycolic Acid and combined with our Step 02 Perfect Grit Priming wand, the system is very effective at removing nail discoloration. Avoiding polish is essential during the treatment period.
Is there anything you can do to prevent polish induced yellowing from happening?
Keeping the canvas healthy is imperative. Over filing the surface can theoretically lead to increase pigment leaching into the nail. Don't forget to use a good quality base coat like the Dr. Dana Hydrating Base Coat unless the product specifies that one is not needed. In most instances, a good quality basecoat will create a protective barrier layer for the nail plate. Lastly, try to remove polish quickly. If you need to rub for 10 minutes then the pigments have a better opportunity to leach into the nail. Quickly remove the polish and wash hands immediately.
Other “non-medical” causes of nail yellowing include staining from extrinsic environmental exposures to ingredients such as tobacco, tanning products or Henna. In these cases a thorough exposure history will usually uncover the yellowing culprit.
There are several causes of nail yellowing that are due to medical conditions. The most common being fungal infections of the nail. Fungal infections of the nail can make the nails thick, yellow, and crumbly. Proper diagnosis and treatment are essential to be able to achieve resolution. Nail fungus (onychomycosis) affects approximately 35 million people in the United States. Fungal nails can be yellow, thick, and crumbly or they can have yellow streaks within the nail plate and be generally smooth and intact. It is far less likely to have a true fungal infection of the fingernails, ie. one that is caused by a dermatophyte. Most toenail fungus starts off in the soft tissue, as athlete’s foot, and then enters the nail when there is an injury or lifting of the nail.
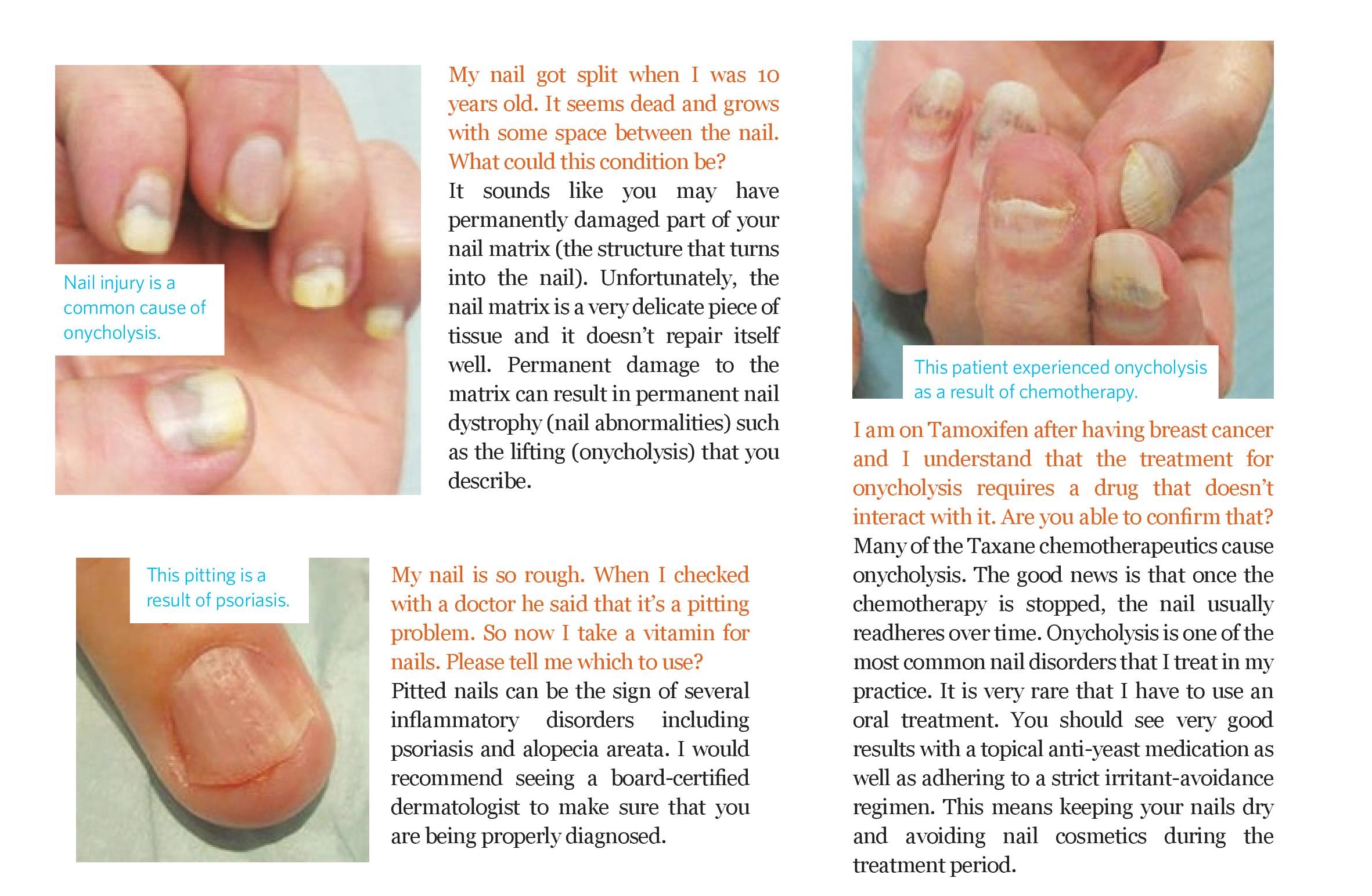
Onycholysis, or separation of the nail plate from the underlying nail bed is another potential cause of nail yellowing. This common condition is often observed on the fingernails in contrast to Onychomycosis where the majority of cases are confined to the toenails. When the nail lifts off of the nail bed, the nail will appear as a white to yellow opacity in the area of separation. This is due to air and other debris under the compromised nail plate. Although there are many causes, the most common include overly aggressive cleaning under the nail as well as some inflammatory conditions such as psoriasis. When the nail is separated, yeast often colonize on the nail bed as it is a barrier compromise that is allowing water and moisture to settle under the nail and these are the ideal conditions that allow yeast to flourish. Treatment will usually include adhering to a strict irritant avoidance regimen where nail polish remover and exposure to household chemicals and water is avoided. Polish removers are strong solvents that will cause irritation to the delicate nail bed tissue when there is an opening under the nail plate. Additionally, a prescription topical anti-yeast treatment will often need to be prescribed.
The Yellow Nail Syndrome is another non-cosmetic cause of nail yellowing. The toenails appear thick and have a yellow to green tinge and frequently lack a cuticle as well as lunula (the half moon that is usually visible on the thumb nail and great toenail). This entity is due to failure of the nail to grow sufficiently and is associated with lymphatic disease as well as lung disease or malignancy. The underlying disorder must be treated but tends to be chronic.